Pan-Retinal Photocoagulation
Diabetic retinopathy does not usually impair sight until the development of long-term complications, including proliferative retinopathy, a condition in which abnormal new blood vessels may rupture and bleed inside the eye. When this advanced stage of retinopathy occurs, pan-retinal photocoagulation is usually recommended.
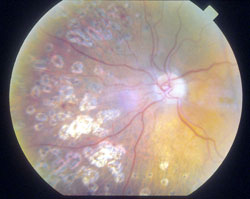
During this procedure, a special laser is used to make tiny burns that seal the retina and stop vessels from growing and leaking. Hundreds of tiny spots of laser are placed in the retina to reduce the risk of vitreous hemorrhage and retinal detachment. Targeted laser applications can treat specific areas in the central vision that are leaking. The laser is used to destroy all of the dead areas of retina where blood vessels have been closed. When these areas are treated with the laser, the retina stops manufacturing new blood vessels, and those that are already present tend to decrease or disappear.
The goal of pan-retinal photocoagulation is to prevent the development of new vessels over the retina and elsewhere, not to regain lost vision.
Pan-retinal photocoagulation is for those:
- who have been diagnosed with proliferative retinopathy
- whose doctor has determined that pan-retinal photocoagulation is the appropriate treatment for their condition
What to expect on procedure day:
Your treatment will be performed in a specially equipped laser room. It does not require a surgery center. It is usually performed without anesthesia, although some will want a local anesthetic.
Before your procedure begins, an eyelid holder will be placed between your eyelids to keep you from blinking. Next, your ophthalmologist will begin laser treatment with an argon or diode laser. The laser treats the peripheral (outside) and middle portions of your retina. It does not treat the central or macular region because this would likely cause serious loss of vision.
The initial treatment usually consists of approximately 1,500-2,000 spots of laser per eye. This will be done in two or more sessions.
Your vision will be poor immediately after the treatment, but will recover to the pre-treatment level over time. You should plan to have someone drive you home, and you should relax for the rest of the day. Most patients resume activities within a few days. Regular follow-up visits are required.
Expectations:
The goal of pan-retinal photocoagulation is to prevent the development of new vessels over the retina and elsewhere, not to regain lost vision. There is no improvement in vision after the laser treatment. Vision may decrease due to edema/swelling of the retina, after the laser treatment. It may improve to its previous level in two to three weeks or may remain permanently deteriorated. Recurrences of proliferative retinopathy may occur even after an initial satisfactory response to treatment.
This procedure sacrifices peripheral vision in order to save as much of the central vision as possible and to save the eye itself. Night vision will be diminished. After pan-retinal photocoagulation, blurred vision is very common. Usually, this blur goes away, but in a small number of patients some blur will continue forever.
Serious complications with pan-retinal photocoagulation are extremely rare, but like any surgical procedure, it does have risks. These risks can be minimized by going to a specialist experienced in pan-retinal photocoagulation.
If you and your doctor decide that pan-retinal photocoagulation is an option for you, you will be given additional information about the procedure that will allow you to make an informed decision about whether to proceed. Be sure you have all your questions answered to your satisfaction.
If you would like more information about this procedure you can make an appointment or contact the office for additional information.


